Earlier this year, Utah passed a law that will directly impact ketamine clinics. The new law is entitled “Anesthesia and sedation requirements – Unprofessional conduct – Whistleblower protection.” Ut. St. § 58-1-510. The new law is effective as of May 4, 2022, but the implementing regulations have been passed or implemented yet. We believe that should happen by November 2022.
The regulations for laws often provide much more detail about how the law will be interpreted and enforced. The regulations tend to “fill in the gaps.” Until the regulations are implemented, there are questions about certain terms and provisions under the new law. In this post, we will describe the new law and how it will impact ketamine clinics in Utah.
As the new law’s title states, there are unprofessional conduct implications for healthcare providers and whistleblower protections. An act of unprofessional conduct by a healthcare provider can lead to severe consequences, including the loss of a license. Whistleblower laws encourage people to come forward when they have witnessed an illegal act.
Often, whistleblower laws are geared toward employees of a company and protect such employees who come forward in good faith to report a violation. Whistleblower laws are quite common in healthcare – it is not uncommon for some of the federal fraud and abuse laws to have whistleblower-type protections.
The basics
The new law describes the requirements for various sedation levels in an outpatient setting. The law (with minor edits) states:
An anesthesia or sedation provider may not cause a patient to undergo moderate sedation, deep sedation, or general anesthesia, in an outpatient setting that is not an emergency department without:
-
first providing the following information in writing and verbally: (i) the level of anesthesia or sedation being administered; (ii) the identity, type of license, and training of the provider who is performing the procedure for which the anesthesia or sedation will be administered; (iii) the identity, type of license, and a description of the training described in Subsection (4) of the anesthesia or sedation provider who will be administering the anesthesia or sedation; and (iv) a description of the monitoring that will occur during the sedation or anesthesia, including descriptions related to the monitoring of the patient’s oxygenation, ventilation, and circulation;
-
after complying with Subsection (2)(a), obtaining the patient’s written and verbal consent regarding the procedure;
-
having the training described in Subsection (4);
-
directly supervising the patient;
-
if the patient is a minor, having a current pediatric advanced life support certification;
-
if the patient is an adult, having a current advanced cardiovascular life support certification;
-
having at least one individual in the procedure room who has advanced airway training and the knowledge and skills to recognize and treat airway complications and rescue a patient who entered a deeper than intended level of sedation;
-
having access during the procedure to an advanced cardiac life support crash cart in the office with equipment that: (i) is regularly maintained according to guidelines established by the American Heart Association; and (ii) includes: (A) a defibrillator; (B) administrable oxygen; (C) age appropriate airway equipment; (D) positive pressure ventilation equipment; and (E) unexpired emergency and reversal medications including naloxone for opioid sedation and flumazenil for benzodiazepine sedation;
-
using monitors that meet basic standards set by the American Society of Anesthesiologists and continually monitoring ventilatory function with capnography unless precluded or invalidated by the nature of the patient, procedure, or equipment; and
-
entering appropriate information into the patient’s chart or medical record, which shall include: (i) the patient’s name; (ii) the route and site the anesthesia or sedation was administered; (iii) the time of anesthesia or sedation administration and the dosage; (iv) the patient’s periodic vital signs during the procedure; and (v) the name of the individual who monitored the patient’s oxygenation and ventilation.
That is a lot to unpack. However, certain aspects are noteworthy. As required under Sections “a” and “b”, above, a provider’s informed consent forms will need to be updated. The law requires both verbal and written informed consent. And the law specifies what must be discussed with a patient prior to starting the procedure.
The law likewise requires (a) the healthcare personnel to have certain training, (b) direct supervision of the patient, and (c) “having at least one individual in the procedure room who has advanced airway training and the knowledge and skills to recognize and treat airway complications and rescue a patient who entered a deeper than intended level of sedation.”
Given these new requirements in Utah, there is now a question about whether telehealth ketamine services can be provided in Utah. For example, the law is focused on “an outpatient setting that is not an emergency department.” Unfortunately, the law does not define an “outpatient setting”. But, given the broad intent of this law, the regulations may, in fact, define an outpatient setting to include telehealth. As of now, we just don’t know what the new regulations will state or require and how they will impact ketamine clinics.
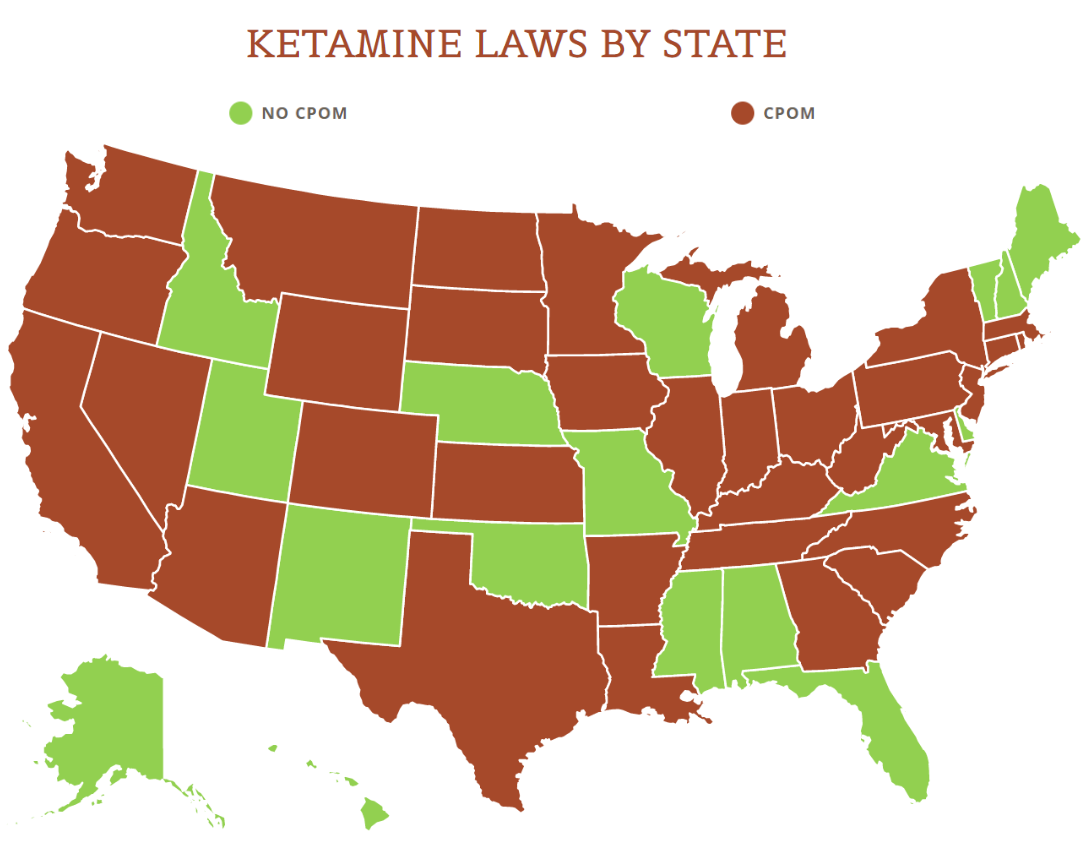
View the US Map of Ketamine Legality
The definitions
Like any new statutory regime, the definitions here are vitally important. Some of the important definitions (with minor edits) include:
“Anesthesia or sedation provider” means an individual who is licensed: (i) under the Podiatric Physician Licensing Act; (ii) as an advanced practice registered nurse; (iii) under the Utah Medical Practice Act; (iv) under the Utah Osteopathic Medical Practice Act; or (v) as a dentist under the Dentist and Dental Hygienist Practice Act, and who has obtained the appropriate permit to administer anesthesia.
“Deep sedation” means a drug-induced depression of consciousness where an individual: (i) cannot be easily aroused; (ii) responds purposefully following repeated or painful stimulation; (iii) may not be able to independently maintain ventilatory function; (iv) may require assistance in maintaining a patent airway; and (v) usually maintains cardiovascular function.
“General anesthesia” means a drug-induced loss of consciousness where an individual: (i) cannot be aroused, even by painful stimulation; (ii) is often unable to maintain ventilatory function; (iii) often requires assistance in maintaining a patent airway and positive pressure ventilation may be required because of depressed spontaneous ventilation or drug-induced depression of neuromuscular function; and (iv) may not be able to maintain cardiovascular function.
“Minimal sedation” means a drug-induced state where an individual: (i) responds normally to verbal commands; (ii) may have reduced cognitive function and physical coordination; and (iii) maintains airway reflexes, ventilatory function, and cardiovascular function.
“Moderate sedation” means a drug-induced depression of consciousness where an individual: (i) responds purposefully to verbal commands, either alone or accompanied by light tactile stimulation; (ii) maintains a patent airway; (iii) maintains spontaneous ventilation; and (iv) usually maintains cardiovascular function.
That is another mouthful and a lot of information to digest. The level of sedation varies from minimal sedation through and including general anesthetics. Likewise, depending upon the level of sedation, the law may or may not apply. If the sedation is moderate, deep, or a general anesthetic, then the new law is triggered.
Thus, the operative question for ketamine providers is whether the level of sedation is minimal. If not, then such providers will need to comply with the new law. Providers at ketamine clinics will need to make these decisions and have a solid basis to back up their decisions if they determine ketamine is a “minimal sedation” procedure. Otherwise, they will run the risk of “unprofessional conduct” which can carry very severe consequences.
The type of provider who administers ketamine is likewise an important aspect of this law. If the provider is a physician, dentist, podiatrist, or advanced practice registered nurse, the law applies to such providers. Presumably, this is the full list of healthcare providers that are allowed to prescribe and administer ketamine in Utah.
Whistleblowers and penalties
The law does not go into detail about violations, other than to note it is an act of unprofessional conduct. The various healthcare professional boards will therefore need to determine the appropriate level of discipline if a provider violates this law. The law states:
An anesthesia or sedation provider who violates Subsection (2) [which is set forth above] or any rule created by the division to implement this section commits unprofessional conduct. Moreover, an individual commits unprofessional conduct if the individual administers anesthesia or sedation for which the individual is not appropriately trained.
One thing noted above is that the new regulations will likewise play an important role. If a provider violates the forthcoming rules, it will be considered an act of unprofessional conduct.
When it comes to whistleblower protections, the law states:
An employer may not take adverse employment actions against an employee if: (a) the employee notifies the division of: (i) a violation of this section; or (ii) a violation of any rule created by the division to implement this section; and (b) the employment action is based on the individual notifying the division of the violation.
The protections will encourage employees to come forward when there has been a violation of the law or the regulations. In fact, the law specifically states that if the “employment action” is based on a report by the employee, the employer cannot take adverse action against the employee.
While this provision seems powerful, the question will be what are the “teeth” to enforce this law? If an employer nonetheless wrongfully terminates an employee for reporting a violation, what will the penalties be for the employer? Will there be monetary penalties? Will there be other types of penalties? We will just have to wait and see what the new regulations state.
Concluding remarks
This is a commonsense law. Any individual undergoing sedation should be afforded basic healthcare protections. While hospitals have very strict laws, guidelines, accreditation standards, and the like, the same is often not true for an outpatient clinic. This new law seems to help bridge the gap.
While some states have similar type requirements for sedation (for example, North Carolina has a similar requirement for nurses; see North Carolina Board of Nursing Review – September 2018; where a registered nurse can give sedation if certain requirements are met), it would not be surprising if other states follow suit and implement similar laws.
But, as noted above, there are many questions that are still unanswered in Utah. When the final Utah regulations are released, we will comment on the new rules. However, in most rulemaking settings, the public is entitled to provide feedback and questions about any proposed or interim rules. If that is available in Utah, ketamine providers would be wise to pay close attention to any such proposed or interim rules.